Families Can Count on Florida KidCare
 If your family no longer qualifies for Medicaid, the Florida Department of Children and Families will automatically share your information with Florida KidCare.
If your family no longer qualifies for Medicaid, the Florida Department of Children and Families will automatically share your information with Florida KidCare.
You can count on Florida KidCare for quality, low-cost health and dental insurance made just for kids – with benefits ranging from doctor visits to surgeries, and so much more.
Be on the lookout for a yellow-striped envelope for more information and next steps. Have questions about how the process works? We're here to help. Visit our frequently asked questions below.
In the meantime, visit www.myflorida.com/accessflorida to update your Medicaid information. The Florida Department of Children and Families may ask for additional information from you while your case is being reviewed.

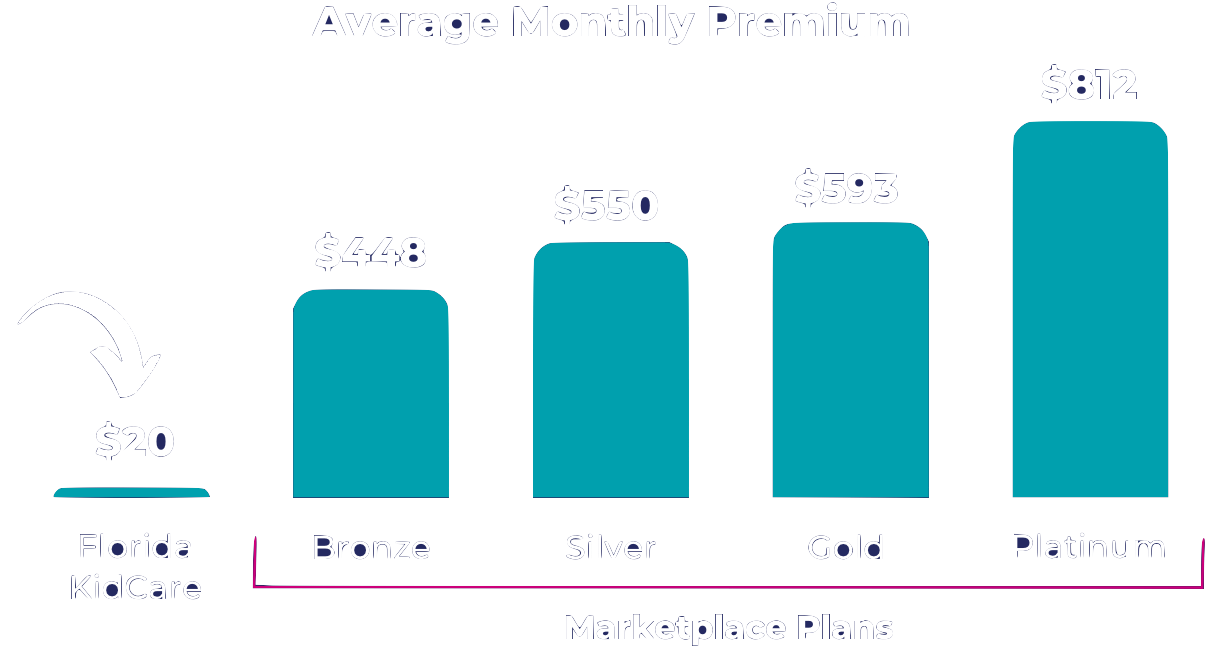
Affordable Coverage
Florida KidCare offers low-cost health insurance options based on the age of the child, and household income and size. Many families pay just $15 or $20 a month to cover all children in the household. See how Florida KidCare stacks up against federal marketplace plans:
Serving Florida families for over 20 years, Florida KidCare matches children with the best plan for their unique needs – given their age, health and more.
Want to talk with someone about all your health insurance options? Find a list of Florida-registered health navigators here.
Health Insurance 101
Don't know how health insurance works? We're here to help! The following short videos provide a basic tutorial on health insurance, and the options and benefits available to your family.
Health Insurance 101:
What You Need to Know
Choosing a Health Plan:
What to Consider
The Cost of NOT Having
Health Insurance
Quality Benefits
Florida KidCare was designed specifically with kids in mind, giving them access to the health services they need at each stage of growth and development.
Benefits include, but are not limited to:
Frequently Asked Questions
1-888-540-KIDS (5437)
TTY 1-800-955-8771
